Abstract
Introduction: Hematological patients as immunocompromised hosts are vulnerable to severe COVID-19 infection. Given the significant risk of heightened morbidity and mortality from COVID-19, there is an urgent and critical need to establish its impact in these population. A better understanding of adverse prognostic factors could assist hematologist to tailor appropriate treatment. With this background, our aims were to analyse the outcome of COVID-19 infection and to identify risk factors associated with severity and mortality.
Methods: This is a multicenter retrospective observational study with data collected from 6 Malaysian hematological centers. This cohort included patients age ≧ 15 years with hematological diseases who developed PCR-documented SARS-CoV-2 infection from 1st January 2021 to 31st December 2021. Data were collected locally from the 6 participating centers. Anonymized data were centrally processed by a coordinating team in Penang General Hospital. The variables assessed included baseline characteristics, type of hematological diseases, anti-neoplastic therapies, COVID-19 treatments and outcomes. Analyses were generated using R statistical software version 4.1.2. Prognostic factors were analysed using Cox proportional hazard regression analysis.
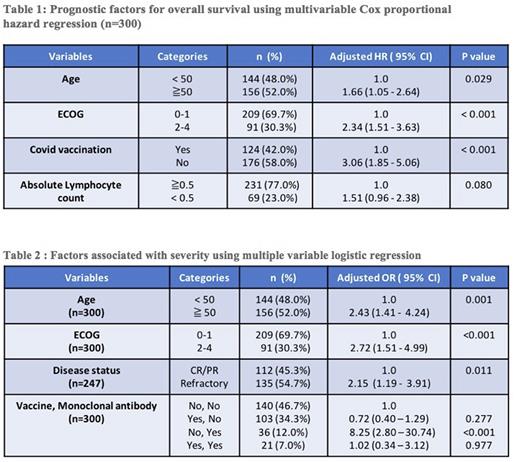
Results: A total of 300 patients (168 males, 132 females) were evaluated. The median age was 51 years (range: 15-85 years). 52% were 50 years old and above. 44% had at least one comorbidity. There were 153 (51%) lymphoid malignancies, 94 (31%) myeloid malignancies and 53 (18%) benign hematological disorders. Non hodgkin lymphoma (26.6%) was the commonest hematological disease followed by acute myeloid leukaemia (16.3 %), acute lymphoblastic leukaemia (9.0%), autoimmune diseases (8.0%) and multiple myeloma (7.0%). Of the 247 patients with malignancy, 55% patients had refractory disease. 104 (42.1%) patients were receiving intensive chemotherapy, 40 (16.2%) low intensity chemotherapy, 25 (10.1%) hypomethylating agent, 22 (8.9%) molecular targeted therapy, 36 (14.6%) supportive care and the remaining 20 (8.1%) were not on active therapy. 19.0% of patients were treated with B cell depleting monoclonal antibody including Rituximab (15.3%), Daratumomab (2.7%) or Blinatumomab (1.0%). Only 24 (8%) patients had prior hematopoietic stem cell transplantation. 34.7% were fully vaccinated prior to COVID-19 infection. 45% of patients developed severe or critical COVID-19 infection based on WHO criteria. Cytokine release syndrome (37%) and organising pneumonia (33%) were the two commonest complications. The median follow up was 158 days (range: 4 - 345 days). The overall mortality rate was 31.7% with survival rate at 90 days of 68.3% (95% CI: 62.6 to 73.2). Poor prognostic factors identified in the multivariable cox regression included age ≥ 50 (HR 1.66; 95 CI 1.05 - 2.64; p = 0.029), ECOG 2-4 (HR 2.34; 95 CI 1.51 - 3.63; p < 0.001), vaccine naive (HR 3.06; 95 CI 1.85 - 5.06; p < 0.001) and absolute lymphocyte count (ALC) < 0.5 (HR 1.51; 95 CI 0.96 -2.38; p = 0.080). Age ≥ 50 (OR 2.43; 95 CI 1.41- 4.24; P = 0.001), ECOG 2-4 (OR 2.72; 95 CI 1.51 - 4.99; p <0.001), refractory hematological disease (OR 2.15; 95 CI 1.19 - 3.91; p = 0.011) and usage of B cell depleting monoclonal antibody (OR 8.25; 2.80 - 30.74; p <0.001) were significantly associated with severe Covid-19 infection.
Conclusion: 45% of hematological patients with COVID-19 had severe or critical infection with mortality rate of 31.7%. Poor survival was correlated with older age (≥ 50 years old), poor performance status, severe lymphopenia and vaccine naive. Vaccination is effective in preventing mortality but not severe infection. Hence, antiviral drugs and anti-SARS COV-2 monoclonal antibodies for early treatment and prophylaxis should also be considered for high risk patients and potential vaccine non-responders.
Disclosures
Tan:Novartis: Honoraria, Research Funding; MSD: Honoraria; Amgen: Honoraria; BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal